
Thanksgiving has become one of the most cherished holidays in the United States, steeped in tradition, gratitude, and shared meals. Its origins are often traced back to the Pilgrims’ harvest celebration in 1621, yet much of what we “know” about that event has been shaped by legend. The historical facts surrounding the first Thanksgiving differ significantly from the modern narrative, which has evolved into a romanticized story of harmony and feasting. Let’s explore what history tells us about that pivotal celebration, examining the number of attendees, the types of food served, the length of the event, and the subsequent creation of the Thanksgiving legend.
The First Thanksgiving
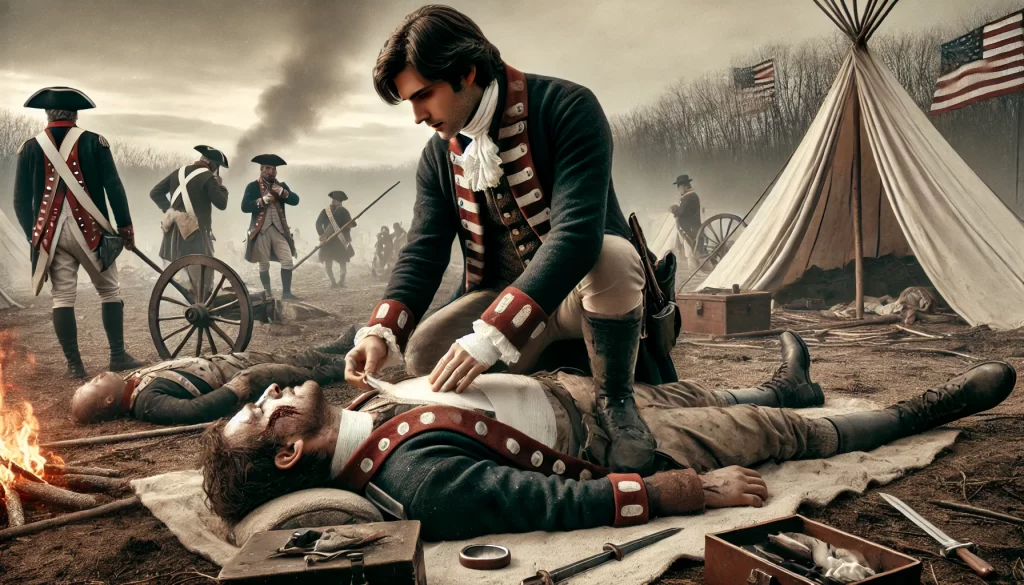
In the autumn of 1621, after a successful harvest, the Pilgrims at Plymouth Colony held a three-day celebration that is often considered the “first Thanksgiving.” This event marked a period of gratitude and alliance-building between the Pilgrims and the Wampanoag people, who were critical to the settlers’ survival during their first year in the New World.
Who Attended?
Approximately 90 Wampanoag men, led by Chief Massasoit, joined 50 surviving Pilgrims for the event. The Pilgrims had arrived aboard the Mayflower the previous year, with 102 passengers. However, disease, harsh conditions, and starvation during the brutal winter of 1620-1621 had decimated their numbers. By the time of the harvest feast, only about half of the original settlers remained. Among the Pilgrims, there were 22 men, 4 married women, and about 25 children and teenagers.
The Wampanoag, who had been instrumental in teaching the Pilgrims essential survival skills, were invited as honored guests.
The Menu
The food served at the 1621 gathering was vastly different from today’s traditional Thanksgiving meal. The feast was primarily prepared by the four surviving adult Pilgrim women: Eleanor Billington, Elizabeth Hopkins, Mary Brewster, and Susanna White. They were assisted by their daughters and four household servants.
While there are no definitive records of the exact dishes, historical accounts and the resources available to the settlers provide clues:
- Meat and Game: The primary protein source was likely wildfowl, such as ducks, geese, and possibly turkey. Deer (venison) brought by the Wampanoag was also a centerpiece.
- Seafood: The Pilgrims relied heavily on the ocean for sustenance, so fish, clams, mussels, and possibly lobster may have been included.
- Grains and Vegetables: Corn was a staple, though it was likely prepared as a simple porridge or bread, not the sweetened dishes we know today. Other vegetables like squash, beans, onions, and native wild plants such as Jerusalem artichokes were likely served.
- Fruits and Nuts: Wild berries, cranberries (unsweetened), and nuts like walnuts and chestnuts may have been part of the feast.
- Beverages: The Pilgrims likely drank water or weak beer, as clean drinking water was not always available.
Absent from the feast were many items central to a contemporary Thanksgiving, such as mashed potatoes, pumpkin pie, and sweetened cranberry sauce. Potatoes and sugar were not readily available, and ovens for baking were primitive at best.
The Celebration’s Length
The first Thanksgiving was not a single meal but rather a three-day event. The Pilgrims and Wampanoag likely engaged in feasting, games, and possibly ceremonial activities. For the Pilgrims, it was a religious occasion, giving thanks to God for their survival and harvest. For the Wampanoag, such feasts were part of their cultural traditions, celebrating seasonal abundance and community.
Myth vs History
As Thanksgiving became a national holiday, myths about the first celebration began to overshadow historical facts. Much of the modern narrative can be traced back to the 19th century, when the holiday was popularized and romanticized.
The Romanticized Myth
The traditional narrative depicts Pilgrims and Native Americans sharing a harmonious meal, much like today’s Thanksgiving dinner. This portrayal emphasizes mutual goodwill and cultural exchange, but it simplifies a far more complex reality
This narrative began to take shape in the mid-19th century when writer Sarah Josepha Hale, editor of Godey’s Lady’s Book, campaigned to make Thanksgiving a national holiday. In 1863, during the Civil War, President Abraham Lincoln declared Thanksgiving a national holiday, emphasizing unity and gratitude. Hale’s writings, along with paintings and school textbooks, reinforced the idyllic imagery of Pilgrims and Native Americans dining together peacefully.
The Historical Complexities
While there was cooperation and mutual benefit between the Pilgrims and Wampanoag during the early years of Plymouth Colony, the relationship was far more complex than the legend suggests. The Wampanoag helped the settlers survive, teaching them to fish and to grow corn in the unfamiliar landscape. However, this alliance was forged out of necessity. The Wampanoag were seeking allies against rival tribes, and the Pilgrims needed help to avoid starvation.
Furthermore, the long-term relationship between European settlers and Native Americans was marked by conflict, displacement, and violence. By the late 17th century, tensions had escalated into King Philip’s War (1675-1678), one of the bloodiest conflicts in colonial American history, leading to the near-destruction of the Wampanoag people. These later events cast a shadow over the harmony celebrated in Thanksgiving lore.
Thanksgiving’s Evolution Over Time
As the centuries passed, the story of this harvest feast evolved into something far removed from its origins.
The mythologizing of Thanksgiving served a broader cultural purpose. During the 19th century, the holiday was framed as a uniquely American tradition, emphasizing family, gratitude, and unity at a time when the nation was deeply divided.
In modern times, Thanksgiving has become a secular holiday centered on food, family, and football, often disconnected from its historical roots. While many still reflect on gratitude, the original religious significance observed by the Pilgrims has largely faded. Similarly, the role of Native Americans in the holiday’s origins is often reduced to a simplistic narrative, overshadowing the complex history of their interactions with settlers.

Reclaiming the Story
In recent years, schools and communities have been actively reshaping the Thanksgiving narrative to present a more accurate and inclusive account of its history. This shift aims to acknowledge the complexities of the holiday’s origins and the experiences of Indigenous peoples.
Efforts have been made to present a more nuanced understanding of Thanksgiving. For example, Native American communities use Thanksgiving as a time for remembrance, marking it as a “National Day of Mourning” to honor ancestors and reflect on the impact of colonization. Educators and historians strive to balance the narrative, acknowledging both the cooperation and conflict between Pilgrims and Native Americans.
Understanding the historical first Thanksgiving as a multi-day harvest celebration shared by two very different cultures can enrich our appreciation of the holiday. By recognizing the complexities of the Pilgrims’ survival and the Wampanoag’s contributions, we can honor the real history while still finding meaning in Thanksgiving as a time for gratitude and reflection.
Conclusion
The first Thanksgiving of 1621 was a far cry from the turkey-laden feasts of today. It was a modest harvest celebration involving around 140 people, featuring wild game, seafood, and native vegetables. The three-day event was as much about survival and diplomacy as it was about gratitude.
Over centuries, this historical gathering has transformed into a powerful national myth that emphasizes unity and abundance. While the legend simplifies and sanitizes a more complex reality, it also reflects the evolving cultural values of the United States. By understanding the truth behind the Thanksgiving story, we can celebrate the holiday with a deeper sense of history, recognizing both its origins and its modern meaning.
Thanksgiving remains a day to give thanks, share food, and connect with loved ones—but it also offers an opportunity to reflect on the broader history it represents.
The most iconic Thanksgiving image.

Sources:
Primary Accounts of the First Thanksgiving:
- Bradford, William. Of Plymouth Plantation. Original accounts describing the Pilgrims’ settlement and their harvest celebration in 1621.
- Winslow, Edward. Mourt’s Relation. An early Pilgrim document providing descriptions of their experiences.
Attendees of the First Thanksgiving:
- Pilgrim Hall Museum. “What Happened in 1621?”
The Menu of the 1621 Feast:
- History Channel. “What Was on the Menu at the First Thanksgiving?”
The Role of Women and Servants:
- New England Historical Society. “The Women Who Cooked the First Thanksgiving.”
- Wikipedia. “List of Mayflower Passengers.”
Evolution of the Thanksgiving Legend:
- Smithsonian Magazine. “The Thanksgiving Myth and What We Should Be Teaching Kids.”
Complex Relationships Between Pilgrims and Wampanoag: Smithsonian Magazine. “The History Behind the Thanksgiving Holiday.”
















The Unprecedented Reach of Social Media
By John Turley
On November 7, 2024
In Commentary
A Vast Reach
Social media has proven to be a more effective platform for spreading propaganda than traditional media due to its vast reach, the ability to target specific users, emotional manipulation, algorithm-driven amplification, and the speed at which information spreads. While print, broadcast, and other forms of media still play roles in shaping public opinion, they simply cannot compete with the scale, focus, and speed offered by social media platforms.
This shift represents a fundamental change in the dynamics of information spread. The power to shape beliefs and influence behavior is no longer concentrated in the hands of a few gatekeepers but is now accessible to anyone who understands how to leverage the tools of technology. As a result, the modern information landscape is more fragmented and volatile, making it increasingly difficult to distinguish between genuine information and propaganda.
Understanding these dynamics is essential for navigating the digital world, particularly as social media plays an ever-larger role in public discourse. Whether we can develop better strategies for recognizing and mitigating propaganda in this new environment remains to be seen, but it must be addressed if we are to preserve the integrity of public information.
Sheer Scale
One of the primary reasons social media is more effective at spreading propaganda than traditional media is its sheer scale. Platforms like Facebook, X (formerly Twitter), Instagram, and TikTok have billions of users globally. Information shared on these platforms can be instantly viewed, and reshared by a wide audience, allowing propaganda to spread virally within hours or even minutes. Unlike print or broadcast media, which require significant resources and distribution channels, social media allows anyone with an internet connection to produce and share content.
Targeting
Another critical advantage social media has over traditional media lies in its ability to micro-target specific individuals or groups. Social media platforms utilize algorithms that gather massive amounts of data on users’ behaviors, interests, and demographics. This data is then used to curate content with which users are most likely to engage, creating a personalized experience. While this system may enhance user satisfaction and increase time spent on the platform, it also can create filter bubbles producing highly effective propaganda.
Propaganda creators can design content that speaks directly to the fears, values, or biases of particular segments of the population. By targeting users who are already inclined to believe certain narratives, propagandists can reinforce pre-existing biases, creating echo chambers in which users themselves specifically choose content that reflects their preexisting ideas without encountering opposing viewpoints.
Emotional Manipulation
Social media platforms are designed to maximize engagement, and the most engaging content is often that which provokes strong emotional responses. Whether it’s outrage, anger, fear, joy, or sadness, emotionally charged content is more likely to be shared and spread than neutral or purely informative posts. This creates an environment in which sensationalism and emotional manipulation thrive, making social media fertile ground for propaganda. The old newspaper dictum, “If it bleeds it leads” has been carried to levels never imagined by previous generations of editors.
The Role of Algorithms
One of the most insidious aspects of propaganda on social media is the role of algorithms in determining what content users see. These algorithms are designed to prioritize content that keeps users engaged, often by promoting material that aligns with their existing beliefs or that provokes strong emotional reactions. In doing so, algorithms contribute to the spread of propaganda by ensuring that polarizing or misleading content reaches more people.
The Speed and Scale of Misinformation
Unlike print or broadcast media, where editorial processes and production timelines can act as natural checks on the spread of misinformation, social media operates in real-time. Users can share content instantly, without fact-checking or verifying sources. This speed makes it much easier for propaganda to spread before it can be debunked. By the time fact-checkers have corrected misinformation, it has already reached millions of people, many of whom may never see the correction.
The decentralized nature of social media makes it difficult to trace the origins of propaganda. Fake accounts, bots, and coordinated campaigns can obscure the sources of misleading content, making it harder for users to assess the credibility of the information they encounter. In traditional media, the source of information is typically clear, whether it’s a newspaper, a television network, or a radio station. On social media, the source of propaganda can be either disguised or entirely anonymous, or perhaps even fabricated by artificial intelligence, adding layers of complexity to the problem.
Hopefully this Brave New World of social media does not overwhelm the values that guide our country.