If you’ve had routine bloodwork lately, you might have noticed something called hemoglobin A1c (or HbA1c) on your results. For years, this test has been the gold standard for monitoring diabetes, but it’s increasingly also being used to assess metabolic health in people who don’t have diabetes. Let’s dig into what this number actually tells us and if lower is always better.
What A1c Actually Measures
Hemoglobin A1c reflects your average blood sugar levels over the past two to three months. When glucose circulates in your bloodstream, some of it sticks to hemoglobin—the oxygen-carrying protein in your red blood cells. The more glucose floating around, the more hemoglobin gets “glycated” (coated with sugar). Since red blood cells live about three months, your A1c percentage gives a rolling average of your blood sugar control. It does not capture individual spikes and dips in glucose, but it correlates reasonably well with overall glycemic exposure and is widely used to monitor diabetes control.
For non-diabetics, a normal A1c is generally considered below 5.7%. The prediabetes range sits between 5.7% and 6.4%, while 6.5% or higher on two separate tests typically indicates diabetes. Nondiabetic adults with A1c above about 6% are more likely to have impaired fasting glucose and other cardiometabolic risk factors than those with A1c around 5.2–5.3%.
These cutoffs represent points where research has shown increased risk for complications, but like most biological measurements, they exist on a spectrum rather than as hard dividing lines.
Even in non-diabetics, A1c can vary by genetics, age, ethnicity, iron levels, sleep quality, and stress—not just diet or exercise. That’s why one person may live at 5.2% with no effort, while another naturally runs 5.6%.
The Prediabetes Gray Zone
Here’s where things get interesting—and a bit complicated. Prediabetes affects roughly 98 million American adults, though most don’t know they have it. An A1c between 5.7% and 6.4% signals that your body’s relationship with glucose isn’t quite right. Maybe your cells are becoming resistant to insulin, or your pancreas isn’t producing insulin as efficiently as it once did. Prediabetes isn’t a disease so much as a metabolic warning sign. It means your body is starting to struggle with glucose regulation—often due to reduced insulin sensitivity, higher visceral fat, chronic stress, poor sleep, or genetics.
The crucial thing about prediabetes is that it’s not a benign waiting room before diabetes. Research shows that even in this intermediate range, you face elevated risks for cardiovascular disease, kidney problems, and nerve damage—though not to the same degree as someone with full-blown diabetes. It often coexists with other metabolic risk factors such as excess weight, dyslipidemia, and elevated blood pressure. A large study published in The Lancet found that people with A1c levels in the prediabetic range had a 15-20% increased risk of cardiovascular events compared to those with normal levels.
The good news? Prediabetes is often reversible. Lifestyle changes—particularly losing 5-7% of body weight through diet and exercise—can bring A1c levels back down. The Diabetes Prevention Program, a landmark study, showed that such interventions reduced the risk of developing diabetes by 58% over three years.
Should Non-Diabetics Aim Lower?
Now we arrive at the million-dollar question: if your A1c is already in the normal range (say, 5.3%), would driving it even lower—to 5.0% or 4.8%—provide additional health benefits?
The honest answer is: we don’t really know, but the evidence suggests probably not much.
Here’s what the research tells us. Population studies have found a continuous relationship between A1c levels and cardiovascular risk even within the normal range, meaning that someone with an A1c of 5.5% might have slightly higher risk than someone at 5.0%. However—and this is critical—this doesn’t necessarily mean that artificially lowering your A1c will reduce that risk. Correlation isn’t causation.
Your A1c reflects your overall metabolic health, dietary patterns, genetics, and lifestyle. Someone who naturally maintains an A1c of 5.0% because they exercise regularly, eat a balanced diet, and have favorable genetics probably has lower risk than someone at 5.5%. But that doesn’t mean the person at 5.5% should obsess over shaving off half a percentage point. Large cohort data suggest that the lowest risk band for nondiabetic adults is roughly an A1c around 5.0–5.6%; below about 5.0% the relationship between A1c and outcomes becomes more complex.
There’s a principle in medicine that “lower is better” but it often has limits. In diabetes treatment, pushing A1c too low can actually increase risks—particularly hypoglycemia (dangerously low blood sugar), which carries its own serious complications. The ACCORD trial, which studied intensive glucose lowering in people with Type 2 diabetes, had to be stopped early because the group targeting very low A1c levels had increased mortality. While this study involved diabetics using medications, it illustrates that extremely low glucose isn’t necessarily optimal.
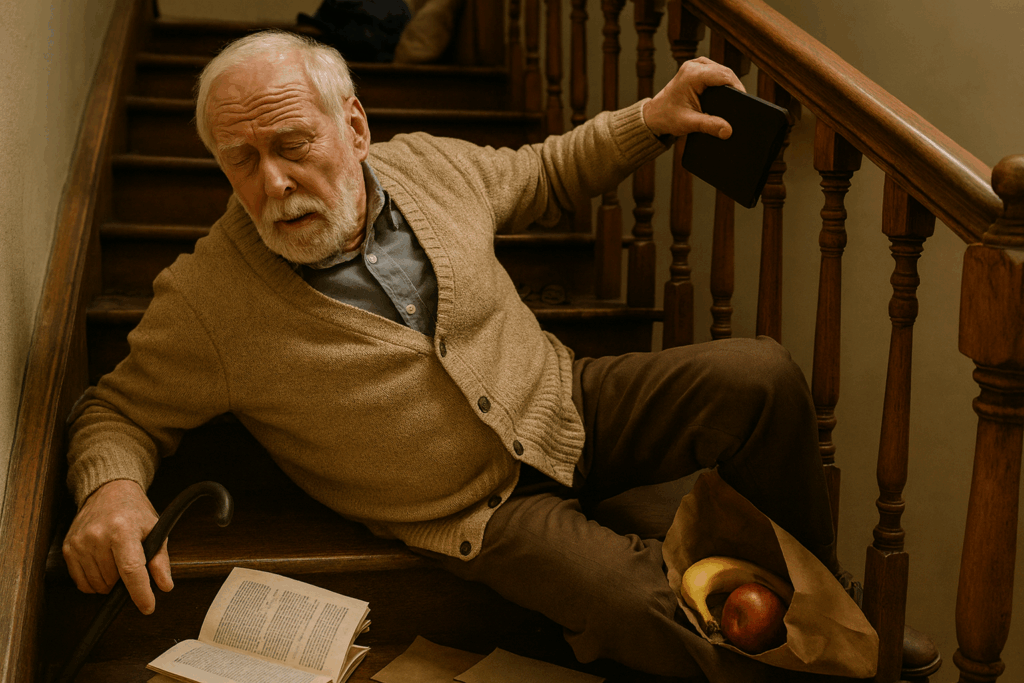
If someone tries to force their A1c unusually low through extreme dieting, fasting, or intensive exercise, they can run into unintended effects such as fatigue and irritability, hormonal disruption, disordered eating patterns, and nutrient deficiencies. Importantly, extremely low A1c values can sometimes reflect anemia or other medical conditions, not superior health.
For non-diabetics with normal A1c levels, there’s no evidence that trying to push numbers lower through extreme dietary restriction or other interventions provides meaningful benefit. Your body is already handling glucose appropriately. The focus should be on maintaining that healthy state through sustainable lifestyle habits rather than chasing incremental improvements in a single biomarker. In practical terms, the benefit is less about the exact number (say 5.1 versus 4.8) and more about maintaining a metabolic profile that keeps A1c comfortably below the prediabetes threshold over the long term
What Actually Matters
Rather than fixating on squeezing every tenth of a point out of your A1c, the evidence supports a broader approach to metabolic health. Regular physical activity, maintaining a healthy weight, eating a diet rich in whole foods with plenty of fiber, getting adequate sleep, and managing stress all contribute to healthy glucose metabolism—and they bring countless other benefits beyond A1c.
It’s also worth noting that A1c isn’t perfect. Certain conditions—like anemia, chronic kidney disease, or hemoglobin variants—can make A1c readings inaccurate. Some people have A1c levels that don’t match what their continuous glucose monitors show, a phenomenon called “glycation gap.” A1c is a useful tool, but it’s one piece of a larger metabolic picture.
The bottom line? If your A1c is in the normal range, you’re doing well. Maintain the healthy habits that got you there rather than micromanaging the number itself. If you’re in the prediabetic range, you have a genuine opportunity to prevent diabetes through lifestyle changes, and bringing that number down has clear benefits. But for those already in the healthy zone, obsessing over fractional improvements likely won’t move the needle much on your actual health outcomes.





The Multitasking Myth
By John Turley
On December 20, 2025
In Commentary, Medicine
What’s Really Happening in Your Brain
You’re probably multitasking right now. Maybe you’re reading this with a podcast playing in the background, or you’ve got three browser tabs open and you’re checking your phone every few minutes. We all do it. We even brag about it on resumes: “Excellent multitasker!” But here’s the uncomfortable truth that neuroscience has been trying to tell us for years—what we call multitasking is mostly an illusion.
What People Actually Mean
When most people say they’re multitasking, they’re describing one of two scenarios. The first is doing multiple automatic activities simultaneously—like walking while talking, or listening to music while folding laundry. The second, and the one that gets more interesting, is rapidly switching attention between different demanding tasks—like answering emails while on a conference call, or texting while watching TV.
The distinction matters because our brains handle these situations very differently. Activities that have become automatic through practice don’t require much conscious attention. You can absolutely walk and chew gum at the same time because neither activity demands your prefrontal cortex’s full attention. But when both tasks require active thinking and decision-making? That’s where things get complicated.
The Brain’s Bottleneck
Here’s what neuroscience tells us: true multitasking—simultaneously processing multiple streams of complex information—is essentially impossible for the human brain. What feels like multitasking is actually rapid task-switching, and your brain pays a price every time it makes that switch.
The limitation comes from something researchers call the “response selection bottleneck.” When you’re performing tasks that require conscious thought, they all funnel through the same neural pathways in your prefrontal cortex. This region can only process one demanding task at a time, so when you think you’re doing two things at once, you’re really just toggling between them very quickly.
Studies using functional MRI brain imaging have shown what happens during this switching process. When people attempt to multitask, researchers observe reduced activity in the regions responsible for each individual task compared to when those tasks are done separately. Your brain literally can’t devote full processing power to both activities simultaneously.
The Switching Cost
Every time you switch from one task to another, there’s a cognitive cost. Your brain needs to disengage from the first task, shift attention, and then reorient to the new task. This happens so quickly—sometimes in tenths of a second—that we don’t consciously notice it. But those microseconds add up.
Sorry, but get ready for some doctor talk. When people switch tasks, imaging studies show increased activation in frontoparietal control and dorsal attention networks, especially in prefrontal regions (like the inferior frontal junction) and parietal cortex (such as intraparietal sulcus). This boosted activity reflects the brain dropping one task set, loading another into working memory, and re‑orienting attention—processes that consume time and neural resources.
Over time, practice can make specific tasks more automatic, reducing average activity in these control networks and allowing smoother coordination of tasks. However, even in trained multitaskers, studies still find evidence for serial queuing of operations in the multiple‑demand frontoparietal network, reinforcing the idea that consciously doing multiple demanding things “at once” is extremely limited.
Research from Stanford University found that people who regularly engage in heavy media multitasking actually perform worse at filtering out irrelevant information and switching between tasks than people who focus on one thing at a time. Essentially, chronic multitaskers become worse at the very thing they practice most.
Even when people train extensively, studies indicate they mainly become faster at switching and coordinating, not truly doing two demanding tasks at once. Experimental work using reaction‑time paradigms shows a reliable “switch cost”: when people change tasks, responses get slower and more error‑prone compared to staying with one task. This cost is one of the strongest signs that most human “multitasking” is serial switching under time pressure rather than genuine simultaneous processing.
The American Psychological Association reports that these mental blocks created by switching between tasks can cost up to 40% of productive time. Think about that for a minute—nearly half your work time potentially lost to the mechanics of jumping between activities.
The Attention Residue Problem
There’s another wrinkle that makes multitasking even less efficient. When you switch away from a task before completing it, part of your attention remains stuck on the unfinished work. Researchers call this “attention residue,” and it reduces your cognitive performance on the next task.
Sophie Leroy, a business professor at the University of Washington, demonstrated this effect in a series of studies. People who switched tasks performed significantly worse on the second task than people who finished the first task before moving on. The unfinished task keeps running in your mental background, using up cognitive resources you need for the new activity.
When “Multitasking” Actually Works
There are legitimate exceptions to the no-multitasking rule, but they’re more limited than most people think. You can successfully combine activities when at least one of them is so well-practiced that it’s become automatic—essentially requiring no conscious thought. You can listen to an audiobook while jogging because your body handles the running on autopilot.
Some research also suggests that certain types of background music or ambient noise can enhance performance on creative tasks, though this seems to work best when the music is familiar and lacks lyrics that compete with language-processing tasks.
Why We Keep Trying
If multitasking is so inefficient, why do we persist? Part of the answer lies in how it feels. Task-switching triggers the release of dopamine, the brain’s reward chemical. Every time you check your phone or switch to a new browser tab, you get a little neurochemical hit. It feels productive, even when it isn’t.
There’s also a cultural element. We live in an attention economy where being constantly connected and responsive feels mandatory. Focusing on one thing can feel like you’re missing out or falling behind, even though the research consistently shows that single-tasking produces better results faster.
It’s worth noting that research consistently shows this gap between perception and performance. People who think they are excellent multitaskers tend to be the worst at it.
The Bottom Line
The evidence is pretty clear: what we call multitasking is really task-switching, and it makes us slower and more error-prone at both activities. Your brain has a fundamental processing limitation that hasn’t changed despite our increasingly multi-screen world. The prefrontal cortex can only fully engage with one complex task at a time, and switching between tasks creates cognitive costs that add up to significant lost productivity and increased mistakes.
This doesn’t mean you should never listen to music while working or that walking while talking will melt your brain. But when you’re doing something that really matters—writing an important email, having a meaningful conversation, learning something new—giving it your full attention will always produce better results than splitting your focus.